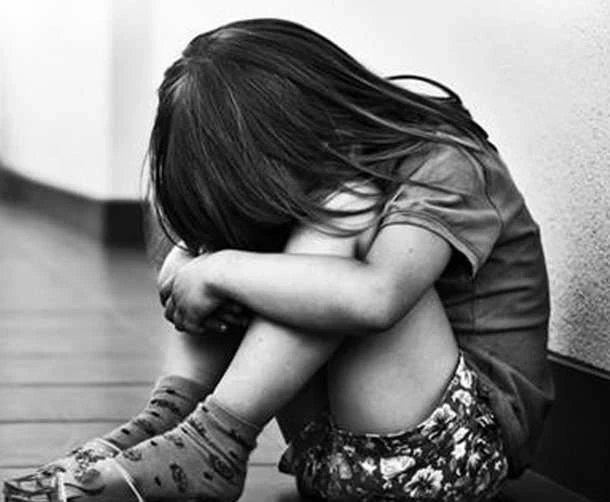
Depression and anxiety are the most common disorders in OECD and EU countries. They have a significant impact on the health and well-being of the population, as well as on the economy as a whole. Are there solutions to combat this problem? EuroNews reports on this.
The report “Strengthening Mental Health and Prevention indicates that about 20% of the adult population in OECD and EU countries suffers from depression. Often, its symptoms go unnoticed and remain untreated, increasing the risk of more serious illnesses and costs to society. The highest prevalence of moderate and severe depression has been recorded in Hungary, Ireland, Italy, Luxembourg, Portugal, and the Czech Republic.
Women are more susceptible to mental disorders during significant moments in their lives, such as pregnancy. According to a study, the rate of postpartum depression is 16.6% in Central and Eastern Europe, 16.3% in Southern Europe, and 13.8% in Northern Europe.
In 2015, the total cost of mental health-related issues was estimated at 4% of the GDP of 27 EU countries and the UK. The costs of treating mental disorders can vary by 20 times depending on the severity of the condition.
According to a German study, in 2019, the cost of treating mental disorders over six months was 511 euros for mild symptoms, 2,417 euros for moderate symptoms, and 10,485 euros for severe symptoms.
The main barriers to seeking help are the high cost of treatment, the need to travel long distances, and long waiting times for appointments with specialists. On average, two-thirds of people in need of psychiatric help remain without access to it in OECD countries and the 27 EU member states.
Initiatives to Improve Mental Health in the EU
Despite this, steps are being taken in several European Union countries to improve access to mental health care, which can significantly reduce the severity and duration of symptoms—by up to 87%.
By the end of 2023, mental health services that can be accessed directly, without a referral, were established in 14 out of 27 EU countries.
In the Netherlands, for example, the @Ease program has been implemented, aimed at training students and frontline professionals to assist young people with mental disorders.
In Belgium, access to psychiatric care has been expanded through partial or full reimbursement of psychotherapy costs, as well as the establishment of networks of mental health specialists in educational institutions, workplaces, and social services.
These measures have contributed to increased school attendance and reduced absenteeism at work—according to available data, this figure ranged from 50% to 61%. Other initiatives include screenings for postpartum depression in Poland and online tools for improving mental health in Germany.