The center actively participates in the implementation of a five-year Roadmap aimed at developing mountainous regions. A distinctive feature of this institution is that Academician M. M. Mirrahimov trained many qualified specialists, creating one of the best schools in cardiology and therapy, which continues the tradition of preparing a new generation of medical personnel, providing accessible and quality medical care.
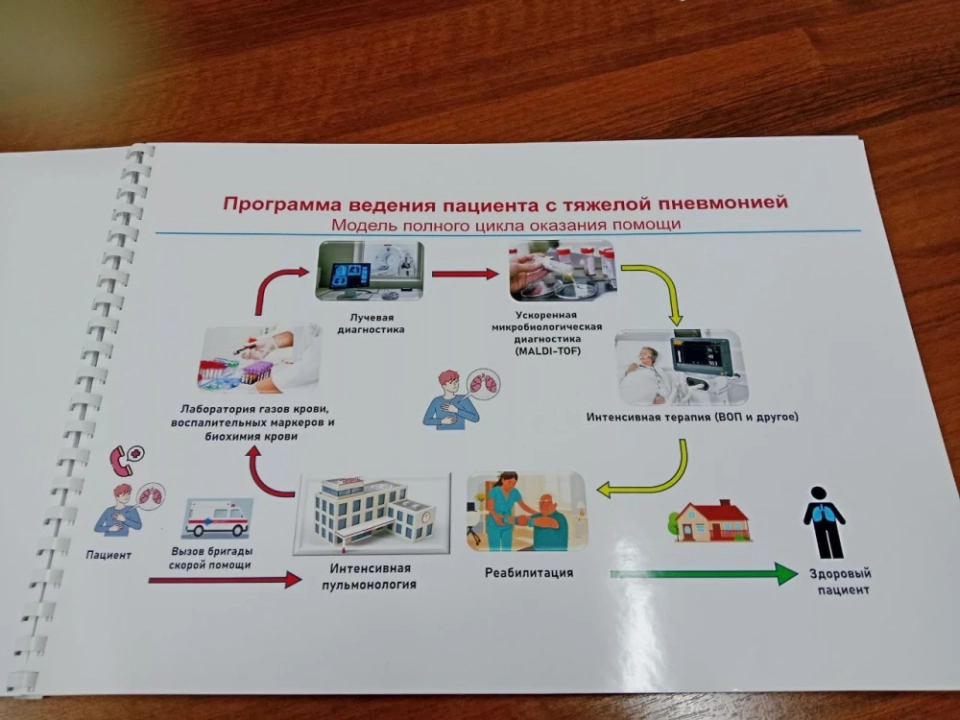
This is of great importance because it was here, when Mirsayid Mirhamidovich headed the center, that modern methods of diagnosing and treating dangerous diseases began to be developed. An integrated approach is what is needed in our time, as patients often suffer from multiple diseases simultaneously. One of the main directions of our center is the creation of effective prevention and treatment programs that take into account multiple pathologies.
We have accumulated significant experience in this field, conducting scientific research and developments.
Our center also stands out as one of the leading scientific institutions not only in the post-Soviet space but also on the international stage. Every year, our specialists publish more than 20 articles in English in the most authoritative global journals. For example, Academician Aldashev became one of the first authors to publish an article in the journal Nature, which has one of the highest impact factors in the world.
Our doctors, especially the younger generation of specialists, are published in journals such as Lancet, Chest, and other reputable English-language publications. This is important, as the development of medicine is impossible without scientific research, and one of the priorities is integration into the international medical scientific community. Academicians Mirrahimov, Aldashev, and other outstanding professors created a system where science, clinical practice, and education develop in harmony — this model continues to operate to this day.
At present, our center has reached a new level in organizing medical care by implementing high technologies and artificial intelligence. We are actively developing these areas.
Our new concept of scientific development includes two key aspects. The first is the formation of scientific clusters consisting of young scientists who are proficient in English. This is essential, as access to current scientific data and integration into the international academic environment is impossible without knowledge of this language.
Each participant in the cluster has undergone training at leading foreign institutions and now conducts advanced research together, including issues related to pneumonia. They are proficient in modern diagnostic and research methods, which creates a foundation for implementing the latest global developments into practice.
It is worth noting that 38 young scientists and doctors from our center are active members of the American College of Cardiology.
The second direction is the creation of a consortium of scientific institutions. We have united seven major medical centers in Kyrgyzstan for the joint development of science and medicine.
Positive changes are already beginning to yield results.We strive to become part of the international scientific and educational network, which is the only right path to the development of science and healthcare as a whole.
Collapse
It is important to understand what "life-threatening disease" means and why panic is inappropriate here.
What is pneumonia? It is an acute infectious-inflammatory process occurring in the respiratory pathways of the lungs. Our respiratory organs consist of two parts: the airways and the respiratory part, where gas exchange occurs. The main function of the lungs is to remove carbon dioxide and saturate the body with oxygen.
Pneumonia affects the respiratory part, where the alveoli are located — the lung sacs through which oxygen enters the blood.During inflammation, the alveoli fill with fluid, disrupting gas exchange. If a significant volume of lung tissue is affected, the patient may develop respiratory failure, which means a lack of oxygen.
The COVID-19 pandemic demonstrated to the whole world what severe pneumonia is. Many patients faced oxygen deficiency. If a large part of the lungs is affected, the remaining part cannot compensate for the deficiency, leading to hypoxia and serious complications, up to death. Therefore, pneumonia should be treated with due attention, and medical standards and recommendations should be strictly followed.
However, there is no need to fear pneumonia, as it is well treatable.There are various clinical forms of pneumonia, some of which are difficult to treat, but overall, the disease is amenable to therapy. The earlier the disease is detected, the higher the likelihood of a successful outcome.
Pneumonia is an acute infectious disease of the lungs. It was previously thought that it is mainly caused by bacteria. However, after the COVID-19 pandemic, doctors realized that viruses can also be responsible, and some viral forms of pneumonia can spread rapidly through the lungs. Some patients experienced damage to up to 90% of lung tissue, but even such complex cases ended in recovery.
Our center conducted the first major study in the country, named COORDINATE, in collaboration with the Copenhagen University Hospital and colleagues from the Department of State Sanitary and Epidemiological Surveillance. The results showed that the main bacterial pathogen of pneumonia in Kyrgyzstan is pneumococci, which corresponds to international data.
This is critically important for doctors, especially in the regions, to correctly determine the treatment strategy and prescribe the necessary antibiotics even without microbiological analysis.
Now they will know which strains of pneumococci are prevalent here and how they respond to antibiotics.We hope to complete this work soon and create a national guideline for the treatment of pneumonia based on the collected data on antibiotic resistance.
Also, during the study, Haemophilus influenzae and Moraxella were identified as other causes of pneumonia. This was established through microbiological analysis of 300 patients. It is important to know which specific bacteria cause pneumonia in Kyrgyzstan and how to treat them correctly, taking into account their resistance to antibiotics.
A small percentage of pneumonias are caused by Staphylococcus aureus, Pseudomonas aeruginosa, and Klebsiella — dangerous microorganisms that are often resistant to antibiotics, leading to severe forms of the disease.
We have already discovered several strains of bacteria in Kyrgyzstan with high resistance to available antibiotics.Fortunately, there are currently not many such strains. The whole world is concerned about the possibility of antibiotic-resistant bacteria emerging, which is associated with their uncontrolled prescription and intake. We often prescribe antibiotics unnecessarily.
Now is the season for ARVI and flu, and there is again excessive prescription of antibiotics to patients with viral infections.The reason is that many patients demand antibiotics, fearing complications. Unfortunately, doctors often prescribe antibiotics when patients come with symptoms of acute respiratory illness, such as high fever and cough.
Doctors are concerned about possible complications.Their fear is quite justified, as there are no rapid methods to determine the need for antibiotic prescription. We are implementing an innovative method that will help doctors make more informed decisions and reduce the number of unjustified antibiotic prescriptions. The device determines the presence of inflammatory signs related to bacterial infection from a finger blood test in just a few minutes, which will help combat the problem of antibiotic resistance.
Our research also revealed that the main viruses causing pneumonia are the influenza virus, adenoviruses, respiratory syncytial virus, rhinoviruses, and metapneumovirus, with a frequency of up to 24.6%. It is important to know this, as antibiotics are ineffective in viral pneumonia, and a different treatment approach is required.
About 20% of cases consist of mixed infections, where both viruses and bacteria are present simultaneously, for example, pneumococcus and rhinovirus.
Understanding the etiology of pneumonia in a specific patient is of great importance.
Antiviral drugs are a complex issue. There are no effective drugs for all viruses; for example, there are none for adenovirus. However, there are antiviral agents with proven efficacy for the influenza virus, recommended in international guidelines.
The main principle for clinical decisions: any medical recommendation should be based on scientific data and supported by research results. The results of our COORDINATE study are published in the prestigious journal THE LANCET and will help create an effective algorithm for treating patients with pneumonia. The citation index of this study is rapidly growing.
Evidence-based facts help us improve clinical practice and, consequently, treat patients with pneumonia more effectively.Pneumonia can also be caused by atypical microorganisms. In our study, Mycoplasma pneumoniae was isolated from 15% of patients, a bacterium that does not have a typical cell wall.
Now we know which pathogens of pneumonia are most common. All results were confirmed in the laboratory of the University of Copenhagen, and we are currently studying the resistance of pneumococci to antibiotics.
This emphasizes that commonly used antibiotics may be ineffective, and if we do not stop the reproduction of bacteria, the disease will progress, leading to serious consequences.
Therefore, it is necessary to remember: "We must preserve antibiotics" and "Be careful with antibiotics." These are chemicals, and improper use can lead to allergic reactions and other side effects, including anaphylactic shock.
We must save antibiotics for those who truly need them.- How to distinguish pneumonia from other respiratory diseases?- Symptoms of pneumonia can resemble other acute respiratory viral infections: cough, fever, sputum production, and general weakness. If you notice these symptoms, you should suspect pneumonia and consult a doctor. If you have shortness of breath, this is a serious reason to seek medical help. Every family, especially during epidemics, should have a pulse oximeter to monitor saturation.
If saturation is below 93%, be sure to call a doctor. Normal values are 91-92%.- How to protect yourself?
- Viruses spread quickly, especially during the epidemic season. It is important to wear a mask and minimize contact with sick individuals, even within the family. This simple but effective rule.
Also, during periods of increased morbidity, it is advisable to avoid large gatherings of people and maintain a healthy lifestyle: proper nutrition, physical activity. And, taking this opportunity, I recommend all smokers to quit smoking, as smoking negatively affects immunity. It has been proven that smokers get sick more often and suffer from illnesses more severely. Smoking is one of the main risk factors for developing severe pneumonia. Users of vapes also often develop atypical pneumonia, which is difficult to treat. Alcohol also poses a serious risk.
Director of the National Center of Cardiology and Therapy named after Academician Mirrahimov, Professor Talant Sooronbaev.
In the current epidemic season, if any family member, whether a child or an adult, has a fever, cough, and other symptoms of acute respiratory illness, the first step should be to contact the family doctor. This should be a mandatory step for everyone.
It is recommended to have a pulse oximeter at home. If saturation is normal, there is no reason to panic, but it is still worth discussing the situation with a doctor to clarify the treatment strategy.
It is important to remember that in 90% of cases, such infections are caused by viruses, and antibiotics should not be used immediately. I would recommend not taking antibiotics at all without a doctor's prescription.
"Do not underestimate, but do not be afraid." Professor on the threat of pneumonia.
Should one treat at home or go to the hospital? In Bishkek, there is a large influx of patients at the infectious diseases hospital, the 3rd Children's City Hospital, and other hospitals. For example, a hundred people are brought in, but only about ten require hospitalization. The rest create queues and additional burdens. Therefore, the decision on the need for hospitalization should be made by the family doctor.
In most cases, patients with ARVI can be treated at home without problems.Often, there is no need for any medications. People take many unnecessary drugs, vitamins, and dietary supplements that have no proven efficacy. There are no "miracle drugs" that help with ARVI or pneumonia. These remedies are unnecessary.
The risk of developing pneumonia is higher in children under 5 years old, elderly people, and patients with chronic diseases. Smokers and alcoholics are at high risk, so they should strictly adhere to preventive measures.
Prevention is of immense importance: wash hands, avoid mass gatherings, wear masks, and lead a healthy lifestyle.
Vaccination is one of the most important preventive measures. Currently, the flu vaccination season is ongoing, and coverage should be around 70% for vaccination to be effective. The pneumococcal vaccine is also very important, as pneumococci often cause bacterial pneumonia. Various types of vaccines — Pneumo-13, Pneumo-23, Pneumo-20 — are widely used around the world. In Kyrgyzstan, the issue of vaccination against pneumococcus for pneumonia prevention is still insufficiently developed, but we have included it in the respiratory disease program.
We have developed an integrated prevention model in which vaccination against flu and pneumococcus is one of the key elements. Thanks to vaccination, severe forms of pneumonia can be prevented, saving the lives of thousands of people in at-risk groups.
So, what to do if you get sick
- Stay home, ensure rest, avoid physical exertion and hypothermia, drink plenty of fluids.
- Do not self-medicate, do not take antibiotics and antiviral medications without a doctor's prescription.
- If the body temperature is below 38°C, antipyretics are not required.
- Antipyretics should only be taken if the temperature exceeds 38-38.5°C; routine use is not recommended.
- If the temperature exceeds 38°C, shortness of breath, chest pain, or cough occurs, especially if you belong to a risk group (children, elderly, pregnant, with chronic diseases) — immediately consult a family doctor or call an ambulance.
- If shortness of breath occurs, measure saturation using a pulse oximeter (if available). If saturation is below 92-93%, consult a doctor or call an ambulance — this is an indication for urgent hospitalization.
- Prevent infection of others: isolate the sick person (separate room, separate dishes); wear a mask; wash hands frequently; ventilate the room and conduct wet cleaning; do not go to work or school until full recovery.