In response to the systemic crisis, doctors have created the Association of Family Medicine of Kyrgyzstan to protect the interests of their colleagues and restore the prestige of the profession, which is essential for the further development of healthcare. Kaktus.media spoke with Nurlan Brimkulov, a professor at the Department of Family Medicine and a board member of the Association. The main points of this interview are presented below.
The image of family doctors has significantly deteriorated. Many believe that this field was chosen only by those who were not accepted into more prestigious departments.
Moreover, the government pays almost no attention to family medicine, which exacerbates the crisis. However, this phenomenon is common throughout the entire healthcare system.
The Minister of Health, Erkin Checheybaev, is a knowledgeable and brave person who raises issues about low salaries for medical workers and the need to increase insurance contributions. His statements are not always received positively.
- I believe that most people support increasing salaries for medical workers. But not everyone is ready to do this at the expense of their modest incomes.
- It is important to understand that the figures of 5.44-7.55% are variable. According to WHO data, 50% of these expenses are paid by the population out of their own pockets. If the state does not provide adequate funding, people are forced to sell their last savings when faced with serious health problems. In contrast to Kyrgyzstan, in Germany and the USA, such payments amount to only 5-10%. Thus, the healthcare system in Kyrgyzstan largely depends on private funds.
When the state does not allocate the necessary funds, people are ready to give their last money to survive.- Shadow payments, in my opinion, are more related to hospitals than to the primary level.
- Why do patients come to hospitals with serious illnesses? This happens due to the lack of timely prevention at the primary level. There are no conditions or opportunities for this. People turn to family doctors only when they already need help. Prevention is practically not carried out, and to change this, a doctor must have a decent salary and normal living conditions.
- If salaries increase and conditions improve, how will prevention be organized at the primary level?
- This is a complex and lengthy process. We plan to implement the experience of Kazakhstan. We visited there, and their model of a multidisciplinary team includes a family doctor and three nurses, as well as a psychologist and a social worker. They have a midwife at one-third of a position. That is, it is not just one family doctor.
Unlike us, where the family doctor is often alone, in Kazakhstan there is a sorting system: a medical worker at the entrance directs patients to the necessary specialist. For example, if someone comes for a prescription, they can get it from the nurse. If a patient comes for a vaccination, they go to the procedure room.
If a patient wants a consultation regarding quitting smoking, they are directed to a special prevention room where a nurse works.
Thus, 50-60% of patients receive help from nurses, and only those who need medical assistance go to the doctor.
- What is the role of the psychologist and social worker?
- For example, if a female patient comes to the doctor with complaints about blood pressure, it turns out that she has family problems. In this case, the psychologist and social worker get involved, who can help solve her problems, for example, with housing or children. This helps eliminate the source of stress, which ultimately normalizes the patient's health condition.
Compare the family doctor in Kazakhstan and Kyrgyzstan, where we do not have a team. We have only two nurses provided, and in reality, often there is not a single one. The salaries of medical workers in Kazakhstan are several times higher, and according to our data, family doctors there earn about a thousand dollars.
In one of the CMS, a doctor from Bishkek said that she works in another region, living in a dormitory on weekdays and returning home on weekends. She noted that among their colleagues, there are also doctors from Kyrgyzstan.
Salary is an important aspect, but working conditions are also necessary. For example, a nurse should have her own office and a minimal set of tools to conduct appointments. We saw how in a large family medicine center in Kazakhstan, 21 rooms are organized, where each nurse can receive patients in a calm environment, which significantly increases the statistics of visits.
In Kyrgyzstan, there is also talk about the need to raise the status of nurses so that they can conduct appointments independently. But in practice, this is poorly implemented, resulting in problems with the organization of appointments.
Psychological support is absent in our health system; we only have psychiatrists, whom many are afraid to approach.
Thus, in Kazakhstan, family doctors are freed from unnecessary burdens and can focus on treating those patients who truly need medical assistance. Each doctor has a team of five to six people, and all of them are provided with the necessary working conditions.
Representatives of the Ministry of Health of Kyrgyzstan are studying the Kazakh experience and plan to implement it in CMS No. 6. Although this is a positive step, additional resources, including financial ones, are needed. We also lack psychologists and social workers, and I fear that family doctors will simply be given even more workload. If there are no changes in salaries and working conditions, our doctors will leave. And the positions of psychologists in the Ministry of Health system, as I mentioned earlier, do not exist.
Options are being developed to launch a pilot project.- Let's return to the creation of the new Association of Family Medicine of Kyrgyzstan. What are its main tasks?
- The Association of Family Medicine of Kyrgyzstan (AFMK) has united family doctors, nurses, and representatives of the academic healthcare sector, including teachers from the Departments of Family Medicine of the I.K. Akhunbaev Kyrgyz State Medical Academy and the S.B. Daniyarov Kyrgyz State Medical Institute for Postgraduate Education.
Asel Tenizbaeva, a well-known healthcare organizer and director of Family Medicine Center No. 6 in Bishkek, became the chairperson of the board. Gulnara Sydygalieva, an experienced family doctor and head of the rural health center in Lenin village of Chui region, who previously actively participated in the work of the Association of Family Doctors, was elected as the deputy chairperson. The board also includes representatives from practical healthcare from all regions of Kyrgyzstan, heads of family medicine departments, as well as young family doctors.
The Association is a successor to the public organization "Family Medicine Without Borders," which mainly united teachers and clinical residents of family medicine and contributed to training, organizing conferences, and promoting scientific research in the field of primary medical and social care for many years.
The new Association aims to significantly expand its influence on the healthcare system, raise the status of family doctors and nurses, and restore the important role of the primary level, as mentioned in the Alma-Ata (1978) and Astana declarations (2018) on primary healthcare.
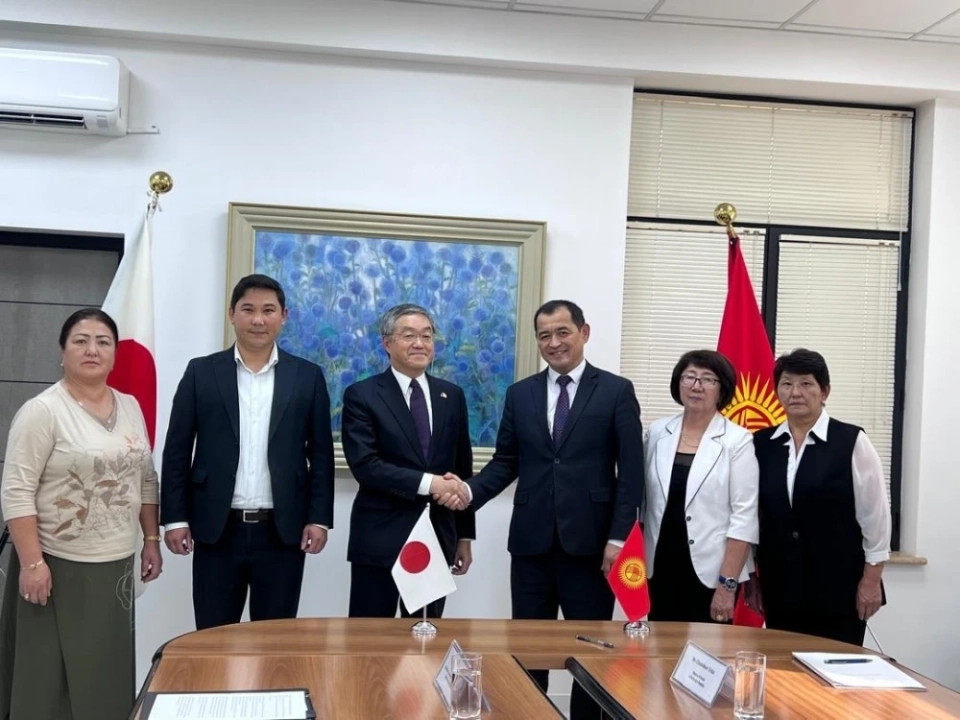
The Association has already begun its work, and its main areas include supporting events for the development of family medicine, educational initiatives, organizing conferences and congresses, participating in the certification of family doctors, as well as providing legal and psychological support for young specialists and developing international ties.
The primary level is the foundation of healthcare, and family medicine is the main driving force at the primary level. This should be reflected not only in words but also in practice, so that doctors feel their significance and importance.
We hope to change the situation of family doctors, improve their working conditions and attitudes towards them, and implement best practices. However, without state support and increased healthcare funding, it will be difficult to achieve changes. The Association will not be able to solve large-scale problems on its own. Without government assistance, the situation will continue to deteriorate, and we may face a situation where even after building new hospitals and purchasing equipment, there will be no specialists left.